This page provides information about the tonsils and adenoids, the reasons surgery may be recommended, risks associated with surgery, and postoperative instructions.
What are tonsils and adenoids and why are they removed?
Tonsils and adenoids are normal tissues which are part of the immune system. Tonsils are located in the back of the throat near the base of the tongue and palate. Adenoid tissue is located in the back of the nose. You can think of the tonsils & adenoids as germ processing centers; they are part of our immune system which helps us fight germs that cause illness. The tonsils & adenoids are only a very small part of our immune system. It turns out that our immune system has many different ways of learning to recognize germs. Children who have their tonsils removed still have a strong immune system and do not have any more illnesses than children who have their tonsils.
The most common reasons for surgery recommendation to remove tonsils and/or adenoids are:
- Recurrent infections
- Chronic infections
- Enlargement of the tonsil and adenoid tissue
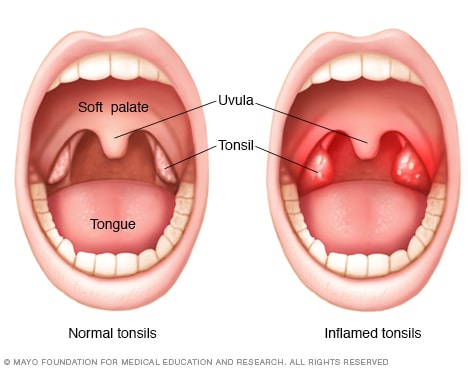
Tonsillitis is inflammation of the tonsils. The inflammation results in sore throat, difficulty and pain with swallowing, fever and frequently changes of the appearance of the tonsils. It can be cause by viral and bacterial infections and the majority will resolve with time, even without antibiotic treatment. When tonsils are infected with a type of bacteria known as Group A Strep, antibiotics are given to prevent complications of the heart and kidneys. When infections occur frequently or are more severe or chronic in nature surgery to remove the tonsils and adenoids may be beneficial.
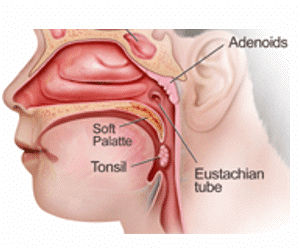
Adenoid and Tonsillar Hypertrophy is abnormal enlargement of the adenoid and tonsil tissue. Hypertrophy may cause problems related to the size of the tissue and problems may include difficulty swallowing, easy gagging, loud snoring or obstruction of the airway (apnea). The significance of the enlargement can sometimes be difficult to establish. Some children with large tonsils and adenoids but no problems related to the enlargement do not need surgery. If symptoms are significant then surgery can be performed to remove the tonsils, adenoids or both depending on the patient’s condition.
Surgery
Removal of the tonsils (tonsillectomy) and adenoids (adenoidectomy) are surgical procedures. They are performed by an ears, nose, and throat surgeon in the operating room under general anesthesia. The goal of surgery is to remove the tissue so that it won’t continue to cause problems from infections or enlargement.
Tonsillectomy -Tonsillectomy is surgery to remove the tonsils. The surgery is done while the patient is asleep. The tonsil is removed from a pocket leaving a small area that heals over the next 1-2 weeks. A tonsillectomy may be performed by itself or at the same time as adenoid removal. Following tonsillectomy patients typically have mild to severe sore throat for 10 to 14 days following surgery. During that time the area where the tonsils were removed is healing and remains very sensitive. This makes it uncomfortable to eat and drink for a while.
Adenoidectomy – Adenoidectomy is surgery to remove the adenoids. The word “adenoids” refers to a single mass of lymphoid (immune tissue) located in the back of the nose and upper throat, near the passage to the middle ear (Eustachian tube). It is hidden from view by the soft palate. Adenoidectomy may be needed if enlarged adenoid tissue obstructs breathing causing nasal obstruction. It may also be done if infected adenoid tissue is thought to contribute to ear infections. An adenoidectomy can be performed alone, with pressure equalization tube placement or with tonsillectomy. Adenoid surgery by itself is typically not very painful.
Most of the time surgery is outpatient, meaning the patient can go home the same day. If children are very young or there is concern for sleep apnea children may be monitored overnight.
Risks of Surgery: Risks are uncommon and include but are not limited to the following
Anesthesia risks. These are related to the process of general anesthesia are extremely rare, your child will be carefully monitored during the procedure. If you have a personal or family history of anesthesia related problems or a history of bleeding problems let your physician know.
Bleeding. This can occur during or after the procedure. It may occur up to 10 days after surgery. Frequently the bleeding stops on its own, sometimes it can be treated in the emergency room, but sometimes the patient will have to go back to the operating room for treatment (especially if they are young).
Dehydration. Since it is painful to swallow, sometimes patients will avoid drinking and become dehydrated. This may require a trip back into the ER or hospital and re-hydration with IV fluids.
Infection
Damage to the teeth, lips, and gums. Surgery is performed in the mouth and rarely the structures of the mouth can be injured from surgical instruments
Velopharyngeal insufficiency (VPI). Normally the palate closes against the back of the throat to prevent food and fluids from entering the nasal cavity. Occasionally after adenoidectomy, the palate has to readjust and patients may have temporary reflux of food and liquids into their nose. Rarely can it be permanent.
Wound problems. These can include scaring, infection, abnormal healing.
Residual disease or recurrent problems. Occasionally problems that we are trying to resolve or improve with surgery persist. Sometimes adenoid tissue can regrow, or sore throats can result from other causes than the tonsils.
Discharge Instructions for Throat Surgery
DIET –The single most important aspect of the patient’s diet in the first three days is adequate fluid intake. Frequent small feedings of soft foods and liquids are usually tolerated best. Make an effort to give drinks every hour during waking hours for the first two days after surgery. Water, jello, yogurt, applesauce, custard, popsicles, Gatorade or Pedialyte are all excellent. Citric acid in juices and carbonation in sodas may burn your throat. As the appetite improves, soft solid foods and chewing are fine; avoiding foods that are tough to chew or will scratch the throat. In general patients can drink anything that feels good. Caffeinated drinks in excess should be avoided because they will cause the patients to lose the fluids. MINIMAL fluid intake for the first 24 hour period is:
| Weight of Patient | Minimal Fluid Intake |
| Over 20 lbs. | 4 cups |
| Over 30 lbs. | 5 cups |
| Over 40 lbs. | 6 cups |
| Over 50 lbs. | 7 cups |
| Over 60 lbs. | 8 cups |
PAIN –Throat pain and/or ear pain is generally quite severe after tonsillectomy and it can take up to 2 weeks for you to feel better. Ear pain frequently occurs between the 3rd and 7th days. The same nerve that goes to the tonsil also goes to the ear and the patient often perceives the pain associated with the tonsillectomy healing as coming from the ear. Following tonsillectomy give regular doses of pain medications 4 to 5 times a day for a week. It will take 30 minutes before it starts to work. Sleeping will be tough. Anti-inflammatory medications such as Motrin, Advil, Ibuprofen, Aleve, and Naproxen Sodium are also frequently used and help reduce pain and inflammation and can be alternated with the other pain medications. Your Surgeon will have prescribed a Pain Medication and it should be used as directed. Further measures to decrease throat discomfort are numbing throat spray, drinking plenty of cool/cold beverages, cool compresses to the neck, ice chips or the use of chewing gum. You swallow 5 times a minute and each and every time will hurt. TAKE THE PAIN MEDICINE AND HYDRATE, HYDRATE, HYDRATE!
BLEEDING –You should have no bleeding from the nose or from the mouth after returning home. There can be abnormal bleeding up to 2 weeks postoperatively. For children, please get up to check the patient once or twice during the first night. If there is blood streaked mucous or saliva try drinking icy slushy liquids and/or gargle with ice chips mixed with water. If this does not stop the bleeding after 30 minutes, call our office during duty hours from M-F at 406-752-8330 to receive further instructions. If you notice any bright red blood, or dark black emesis (vomiting after the first three days) go to the nearest ER.
FEVER –It is normal for patients to run a fever between 99 and 1O1 degrees for the first few days following tonsillectomy. Fever is worsened by a poor fluid intake producing dehydration. For children, fevers also can be reduced by encouraging being more active and taking deep breaths. Taking walks, deep sigh breaths, etc. may help. Tepid (not warm, not cool) bathes may help. Avoiding heavy exercise for all patients will help decrease the chance but not eliminate it.
ACTIVITY –It is advisable to rest at home for the first 48 hours. During this time patients should be up and walking. The more you move around, the sooner you will start to feel better. Activity may be gradually increased as the patient feels better. Normal daily activities can be resumed as the patient tolerates. Vigorous physical activity should be avoided for 14 days following tonsil surgery.
BAD BREATH -Bad breath is quite common. This results from a white to yellowish membrane that forms in the throat in the region of the tonsil surgery. Bad breath may be improved by gargling a mild salt water solution. This may be made by adding 1/2 teaspoon of table salt to 8oz. of warm tap water. The membrane sloughs off during healing between the 5th and 10th days postoperatively and when this occurs the patient may spit up some bloody mucous.
These are common medications used after surgery.
- Tylenol Acetaminophen
Use: Tylenol is used for mild to moderate pain. Tylenol liquid 160mg/5ml is used commonly for children.
Instructions:
Adolescents, and Children >= 12 years: 325—650 mg PO every 4—6 hours, as needed. Alternatively, 1000 mg PO, 2—4 times per day can be given.
Infants and Children < 12 years: 10—15 mg/kg PO every 4—6 hours.
Neonates: 10—15 mg/kg PO or PR every 6—8 hours as needed.
Precautions: Do not exceed 1 g/dose or 4 g/day. - Motrin IbuprofenUse: Motrin is used for mild to moderate pain. Motrin liquid 100mg/5ml is used commonly for children.
Instructions:
Children 1—12 years: 10 mg/kg every 6 hours as needed for pain.
Motrin dosing can be alternated with Tylenol. If children are having more severe pain give a dose of Motrin and Tylenol at the same time.
Precautions: Doses exceeding 50 mg/kg/day are not recommended. - Tylenol with Codeine
Use: Drug combinations of Tylenol and codeine (narcotic) are used for moderate to severe pain. These are often avoided in younger children.